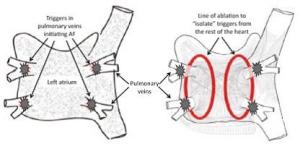
In this procedure, heating energy (radiofrequency ablation) is used to get rid of the triggers that cause AF. In some cases freezing energy is delivered instead (cryoballoon). The triggers that cause AF usually come from the pulmonary veins (tubes that drain blood from the lungs to the heart). The aim of the procedure is to create an electrical barrier (like a road block) so that the electrical triggers can’t get out of the pulmonary veins to start up AF (see below). This procedure is called Pulmonary Vein Isolation (PVI). In some cases of AF ablation is performed in other areas of the heart.
